Click here to launch the Simbryo Head & Neck Development animation (and some really trippy music -you'll understand once the window opens...)
I. Pharyngeal apparatus
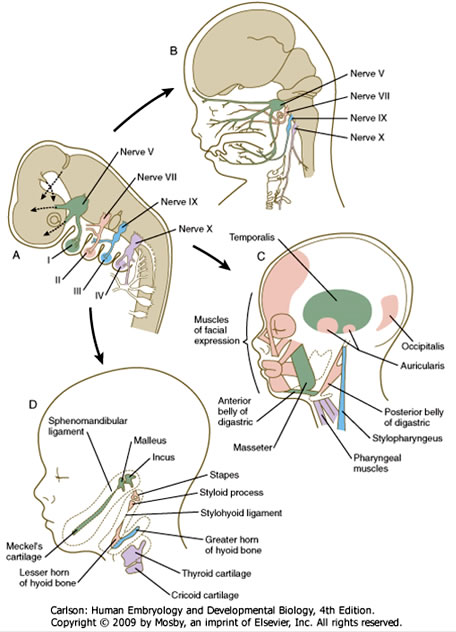
- pharyngeal arches are paired structures associated with the pharynx that contribute greatly to the formation of the face, jaw, ear, and neck
- the 1st pharyngeal arch appears at about the beginning of the 4th week and others are added more caudally later such that there are ultimately 5 arches by the end of the 4th week; the 5th arch fails to form, so the arches are numbered 1, 2, 3, 4, and 6.
- the entire apparatus consists of paired pharyngeal arches, pharyngeal pouches, pharyngeal clefts (or grooves), and pharyngeal membranes (see diagram).
- each pharyngeal arch consists of a core of somatic mesoderm and neural crest mesenchyme
- somatic mesoderm contributes to the arch artery (i.e. aortic arches 1-6) as well as skeletal muscle tissue in each arch
- neural crest mesenchyme develops into bone, cartilage, and/or connective tissue in each arch.
- each pharyngeal arch has a cranial nerve associated with it:
- arch 1: CN V (trigeminal)
- arch 2: CN VII (facial)
- arch 3: CN IX (glossopharyngeal)
- arch 4: CN X (superior laryngeal branch of the vagus)
- arch 6: CN X (recurrent laryngeal branch of the vagus)
- the inside of the pharyngeal apparatus is lined by endoderm that forms infoldings or pouches between the arches; since there are 5 pharyngeal arches, there are 4 pharyngeal pouches, the fates of which are discussed below.
- the outside of the pharyngeal apparatus is covered by ectodermal that forms outer pharyngeal clefts (or grooves); as with the pouches, there are initially 4 pharyngeal clefts, the fates of which are discussed below.


A. Fates of pharyngeal clefts
The pharyngeal clefts are ectodermal-lined recesses that appear on the OUTSIDE of the pharnyx between the arches; cleft 1 is between arch 1 and 2, cleft 2 is between arches 2 and 3, etc.
1. pharyngeal cleft 1: develops into the external auditory meatus (the corresponding 1st pharyngeal pouch develops into the auditory (or Eustacian) tube, and the intervening membrane develops into the tympanic membrane).
Defects in the development of pharyngeal cleft 1 can result in preauricular (i.e. in front of the pinna of the ear) cysts and/or fistulas.
2. pharyngeal clefts 2, 3, and 4 are overgrown by expansion of the 2nd pharyngeal arch and usually obliterated
Remnants of pharyngeal clefts 2-4 can appear in the form of cervical cysts or fistulas found along the anterior border of the sternocleidomastoid muscle.

B. Fates of pharyngeal arches
1. Pharyngeal Arch 1 (mandibular arch)
- associated with the 1st aortic arch, which develops into part of the maxillary artery
- innervated by CN V (trigeminal nerve)
- splits into an upper maxillary prominence and a lower mandibular prominence
- derivatives of the 1st arch are:
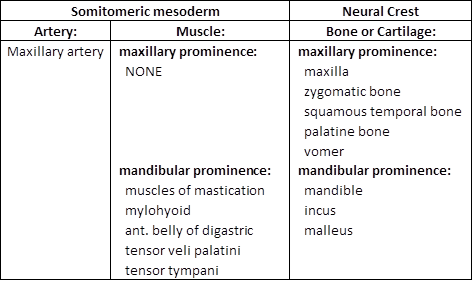
2. Pharyngeal Arch 2 (hyoid arch)
- associated with the 2nd aortic arch, which develops into the stapedial artery
- innervated by CN VII (facial nerve)
- derivatives of the 2nd arch are:
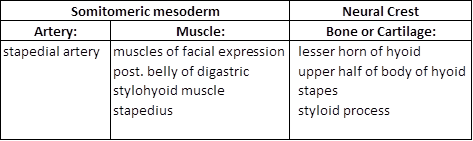
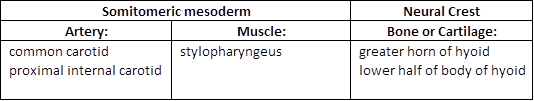
3. Pharyngeal Arch 3
- associated with aortic arch 3, which contributes to the common carotid artery and proximal segment of the internal carotid artery
- innervated by CN IX (glossopharyngeal nerve)
- derivatives of the 3rd arch are:
4. Pharyngeal Arch 4
- associated with aortic arch 4, which contributes to the proximal segment of the right subclavian artery and the arch of the aorta
- innervated by CN X (superior laryngeal branch of the vagus nerve)
- derivatives of the 4th arch are:

5. Pharyngeal Arch 6
- associated with aortic arch 6, which contributes to the proximal segments of the pulmonary arteries and ductus arteriosus (which becomes the ligamentum arteriosum in the adult)
- innervated by CN X (recurrent laryngeal branch of the vagus nerve)
- derivatives of the 6th arch are:

The fates of the pharyngeal arches and their derivative structures can be summarized by the two figures below:

6. Mucles of the head and neck
BRANCHIOMERIC (i.e. in branchial arches – aka pharyngeal arches)
- Arise from unsegmented paraxial mesoderm (i.e. somitomeres) that migrates into arches 1-3:
- Arch 1: muscles of mastication, tensor tympani, tensor veli palantini, anterior belly of digastric (CN-V)
- Arch 2: muscles of facial expression, stapedius, stylohyoid, posterior belly of digastric (CN-VII)
- Arch 3: stylopharyngeus (CN-IX)
- Arise from egmented (somitic) paraxial mesoderm that migrates into arches 4 and 6:
- Arch 4: pharyngeal constrictors, levator veli palatini (superior laryngeal branch of CN-X)
- Arch 6: intrinsic laryngeal muscles (recurrent laryngeal branch of CN-X)
SOMATIC (i.e. NOT in pharyngeal arches)
- Arise from unsegmented paraxial mesoderm that does NOT migrate into arches:
- Extraocular muscles (CN-III, -IV, -VI)
- Arise from somitic paraxial mesoderm that migrates into the tongue after its formation:
- Intrinsic and extrinsic muscles of the tongue (CN-XII)
OCCIPITAL (from occipital lateral plate mesoderm but innervated by a cranial nerve)
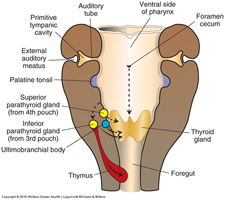
C. Fates of pharyngeal pouches
The pharyngeal pouches are endodermal-lined pockets that form on the INSIDE of the pharynx between the arches; pouch 1 forms between arch 1 and arch 2, pouch 2 forms between arch 2 and arch 3, etc.
 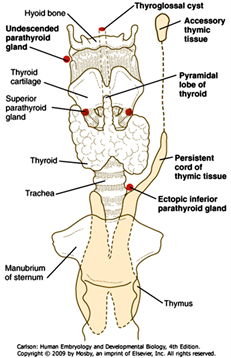
1. Pharyngeal Pouch 1 –develops into the auditory tube and middle ear cavity
2. Pharyngeal Pouch 2 –forms numerous infoldings that become the crypts of the palatine tonsil; later, lymphocytes (from the thymus and bone marrow) infiltrate the underlying lamina propria to establish the definitive palatine tonsil.
3. Pharyngeal Pouch 3 –divides into a superior (or dorsal) and inferior (or ventral) portion:
dorsal portion of pouch 3: forms the inferior parathyroid glands –the chief (or principal) and oxyphil cells are derived from the endodermal lining of the pouch
ventral portion of pouch 3: forms the thymus –the epithelial reticular cells (including those that comprise the thymic or Hassall's corpuscles) are derived from the endodermal lining of the pouch. T-cell progenitors from the bone marrow infiltrate the cortex to establish the definitive thymus.
4. Pharyngeal Pouch 4 –also divides into a superior (or dorsal) and inferior (or ventral) portion:
dorsal portion of pouch 4: forms the superior parathyroid glands –the chief (or principal) and oxyphil cells are derived from the endodermal lining of the pouch
ventral portion of pouch 4: forms a diverticulum called the ultimobranchial body, the cells of which migrate into the thyroid gland and differentiate into parafollicular (C) cells of the thyroid gland.
Anomalous development of the derivatives of pouches 3 and/or 4 can result in ectopic or absent parathyroid, thymic, or parafollicular thyroid tissue. The most common disorder in which this occurs is DiGeorge syndrome, caused by a deletion in the long (or "q") arm of chromosome 22, leading to a hypoplasia of 3rd and 4th pharyngeal arches and their associated phayngeal pouches. Symptoms and signs of DiGeorge often include:
- hypoplasia of the hyoid
- thymic hypoplasia (immunodeficiency due to a lack of T-cells)
- hypoparathyroidism (missing or hypoplastic inferior parathyroid glands)
- outflow tract defects (neural crest in this area also contributes to conotruncal cushions of the outflow tract)
Interestingly, the hypoplasia of the 3nd and 4rd arches can also disrupt the 1st and/or 2nd arches, leading to the following additional findings:
- micrognathia (reduced jaw)
- cleft palate
- hearing loss (either due to malformation of middle ear ocssicles or secondary to ear infections caused by immunodeficiency)
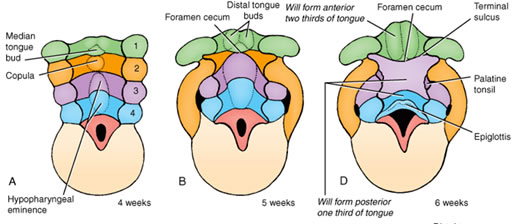
II. Development of the tongue
A. Anterior 2/3 of the tongue:
1. Formation: the anterior 2/3 of the tongue is derived from median and lateral tongue buds that arise from the floor of the 1st pharyngeal arch and then grow rostrally. The tongue buds are then invaded by occipital myoblasts that form the intrinsic muscles of the tongue.
2. Innervation of the anterior 2/3 of the tongue:
- sensory innervation of the mucosa is via the lingual branch of the trigeminal nerve
- taste innervation is via the chorda tympani branch of the facial nerve, except for the taste buds in any circumvallate papilla that may be present in the posteriormost part of the anterior 2/3 of the tongue –these are innervated by the glossopharyngeal nerve.
- motor innervation of the intrinsic skeletal muscles is via the hypoglossal nerve
B. Posterior 1/3 of the tongue:
1. Formation: swellings from the floor of the 3rd and 4th pharyngeal arches overgrow the 2nd arch and fuse with the anterior 2/3 of the tongue. Thus, the posterior 1/3 of the tongue is derived from the 3rd and 4th arches and there is NO contribution of the 2nd pharyngeal arch in the adult tongue. Intrinsic musculature is also derived from occipital myoblasts. The line of fusion of the anterior 2/3 and posterior 1/3 of the tongue is indicated by the terminal sulcus.
2. Innervation of the posterior 1/3 of the tongue:
- sensory innervation of the mucosa is mostly via the glossopharyngeal nerve (and some vagus)
- taste innervation is mostly via the glossopharyngeal nerve (and some vagus)
- motor innervation of the intrinsic skeletal muscles is via the hypoglossal nerve
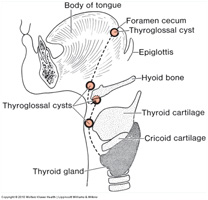
III. Development of the thyroid gland
- is NOT derived from any of the pharyngeal pouches
- arises from a midline thyroid diverticulum that forms from the endoderm in the floor of the pharynx just caudal to the 1st pharyngeal arch; these endoderm cells differentiate into the follicular cells of the thyroid gland.
- endodermal cells of the ultimobranchial body migrate into the gland and give rise to the parafollicular cells (aka C-cells) of the thyroid.
- with differential growth of the embryo, the diverticulum elongates, but remains connected to the forming tongue by a thyroglossal duct that later is obliterated; the site of the opening of the thyroglossal duct is the foramen cecum found in the midline at the terminal sulcus of the tongue.
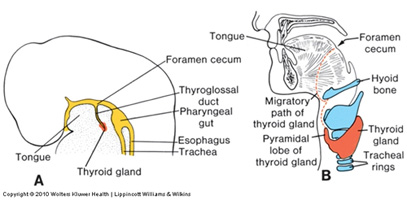 
Anomalies in thyroid development can result in ectopic thyroid tissue and/or cysts present along the course of the thyroglossal duct, which is a midline structure (as opposed to cervical cysts, which are remnants of pharyngeal clefts 2-4 and are found lateral to the sternocleidomastoid muscles).
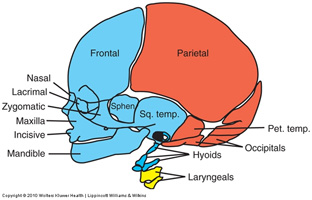
IV. Development of the skull
- anterior portions (viscerocranium) are derived primarily from neural crest mesenchyme that develop into bones via membranous ossification
- bones in the floors of the cranial fossae, aka the "chondrocranium" (cribriform plate, sphenoid, petrous temporal and clivus of the occipital), are derived from paraxial (somitic) mesoderm that develop bone via endochondral ossification
- flat bones of the cranial vault, aka the "neurocranium" (e.g. parietal and posterior occipital), are derived from paraxial (somitic) mesoderm that develops into bone via membranous ossification.
- the hyoid bone is derived from neural crest associated with pharyngeal arches II and III.
- the laryngeal cartilages are derived from neural crest associated with pharyngeal arches IV and VI.
- the bones of the skull do not fuse together until after birth (to allow crowning of the head during delivery and growth of the brain postnatally), leaving sutures and fontanelles that typically close at various times postnatally:
- the confluence of the lambdoid and sagittal sutures at the back of the skull marks the site of the posterior fontanelle, which typically closes at around 3-6 months postnatally
- the confluence of the sagittal, coronal, and frontal sutures at the top, front of the skull marks the site of the anterior fontanelle, which typically closes by 1.5-2 years postnatally.
Because the brain continues to grow in size up until 6-7 years of age, premature fusion of the sutures or fontanelles will result in abnormal shaping of the head as the brain will cause displacement of the bones that remain unfused.
V. Development of the face
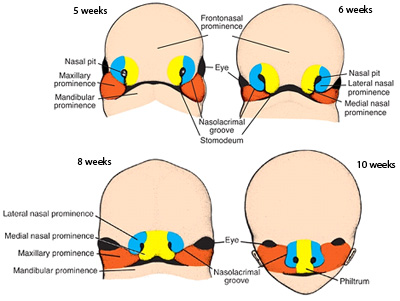
- initially formed by 5 mesenchymal swellings (aka processes or prominences):
- 2 mandibular prominences (right and left, from 1st arch neural crest mesenchyme)
- 2 maxillary prominences (right and left, from 1st arch neural crest mesenchyme)
- frontonasal prominence (midline structure, from cranial neural crest mesenchyme)
- two nasal pits develop in the ventrolateral aspects of the frontonasal prominences, thereby forming 2 lateral and medial nasal prominences
- development of the face occurs via the growth and fusion of these prominences:
- the mandibular prominences grow together to form a single mandible
- The maxillary prominences (shown in orange below) grow toward the midline and fuse with the lateral nasal prominences (blue). A deep groove called the nasolacrimal groove forms between the maxillary and lateral nasal prominences on either side of the developing nose. Most of the groove is obliterated with fusion of the maxillary and lateral nasal prominences, but a small portion persists as the nasolacrimal duct and lacrimal sac.
- Inward growth of the maxillary prominences also causes them to fuse with the medial nasal prominences (yellow). Continued growth of the maxillary prominences combined with regression of the frontonasal prominence pushes the two medial nasal prominences together such the medial prominences eventually fuse to form the midline of the nose and philtrum of the upper lip –the superior portion of the frontonasal prominence grows and extends to form the forehead whereas the inferior portion does not grow very much, thus allowing the medial nasal processes to fuse in the midline.
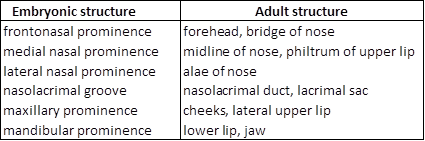
Below is a summary of the contributions of the prominences to the adult face:
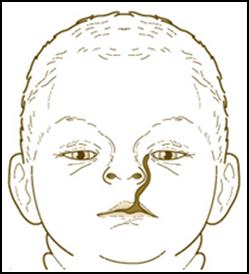
Disruption of the development of any of the facial prominences can result in a variety of facial anomalies, such as (from left to right in figures below):
- hare lip (bilateral failure of maxillary and medial nasal prominences to fuse)
- oblique facial cleft (unilateral failure of maxillary, medial, and lateral nasal prominences to fuse)
- macrostoma (incomplete lateral merging of maxillary and mandibular processes)
- median cleft lip (incomplete fusion of medial nasal prominences)
- frontonasal dysplasia (hyperplasia of inferior frontonasal prominence, thus preventing fusion of the medial nasal prominences)

VI. Development of the palate
A. Primary palate
- forms via the fusion of the two medial nasal prominences in the midline (of course, this midline fusion is driven via growth of the maxillary prominences which pushes the nasal prominences toward to the middle)
- consists of the premaxillary segment of the maxilla, which contains the four incisors and the incisive canal
B. Secondary palate
- forms via outgrowths of the maxillary prominences called the palatine shelves
- initially, the palatine shelves project on either side of the tongue. With growth and expansion of the mandible the tongue moves down, allowing the palatine shelves to grow toward the midline and fuse to form the secondary palate, which consists of the palatine segment of the maxilla and palatine bone. Disruption of growth of the tongue and/or mandible can therefore secondarily cause a cleft secondary palate.

Complete fusion of the primary and secondary palate is a complex process involving growth of the component tissues, epithelial to mesenchymal transformation, cell migration, and programmed cell death at fusion sites –disruption of any part of this process can result in cleft palate. Given the involvement of the maxillary and nasal prominences, cleft palate is often (but NOT always) accompanied by cleft lip.
Practice Questions
1. In craniofacial development, paraxial mesoderm contributes to which of the following?
A. occipital bone
B. muscles of the tongue
C. extraocular muscles
D. NONE of the above
E. ALL of the above
ANSWER
2. The craniofacial defect illustrated in the figure below was most likely caused by which of the following?

- premature fusion of the saggital cranial suture
- premature fusion of the coronal cranial suture
- overgrowth of the frontonasal process
- incomplete fusion of the frontonasal and maxillary processes
- incomplete migration and/or differentiation of cranial neural crest cells
ANSWER
3. The condition shown in the figure below was most likely caused by:
A. failure of the medial and lateral nasal processes to fuse with the maxillary process.
B. incomplete merging of the maxillary and mandibular processes.
C. incomplete fusion of the medial nasal processes.
D. overgrowth of the frontonasal process.
E. incomplete growth of the mandibular process.
ANSWER
4. The thyroid gland is derived primarily from the:
A. 1st pharyngeal pouch.
B. 2nd pharngeal pouch.
C. ventral portion of the 3rd pharyngeal pouch.
D. dorsal portion of the 4th pharyngeal pouch.
E. foramen cecum at the base of the tongue.
ANSWER
5. Which of the following clinical findings is observed more frequently in association with DiGeorge syndrome but not usually in Treacher Collins syndrome?
A. T-cell leukopenia
B. B-cell leukopenia.
C. pharyngeal and/or palatal abnormalities.
D. facial abnormalities.
E. external ear abnormalities.
ANSWER
6. Chromosomal analysis of a patient with DiGeorge syndrome would likely show which of the following?
A. trisomy 21
B. 46, XO
C. deletion of 22q
D. deletion of 11q
E. duplication of 17p
ANSWER
Questions 7-10 refer to the list below. Select the most appropriate structure in the list for each of the following statements or descriptions (each labeled structure may be used once, more than once, in combination with other structures, or not at all). If a statement or description refers to a structure NOT in the list then the correct answer would be "NONE of the above."
A) pharyngeal arch 1
B) pharyngeal arch 2
C) pharyngeal arch 3
D) pharyngeal arch 4
E) pharyngeal arch 5
F) pharyngeal arch 6
7. gives rise to the stapes
ANSWER
8. gives rise to the mandible
ANSWER
9. its derivatives are innervated by cranial nerve III
ANSWER
10. its derivatives are innervated by the hypoglossal nerve
ANSWER
Questions 11-14 refer to the diagram below. Select the most appropriate structure in the list for each of the following statements or descriptions (each labeled structure may be used once, more than once, in combination with other structures, or not at all). If a statement or description refers to a structure NOT in the list then the correct answer would be "NONE of the above."
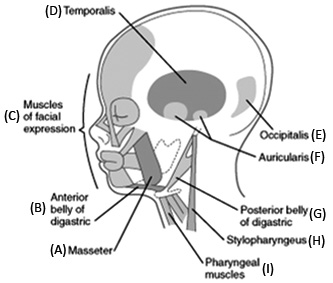
11. innervated by the facial nerve
ANSWER
12. innervated by the vagus nerve
ANSWER
13. innervated by cranial nerve VIII
ANSWER
14. innervated by cranial nerve V
ANSWER
Questions 15-17 are based on the image below showing an 8-year old female and her 6-year old brother.

15. Based on the appearance of these two siblings, which pharyngeal arch appears to be most affected?
A. pharyngeal arch 1
B. pharyngeal arch 2
C. pharyngeal arch 3
D. pharyngeal arch 4
E. pharyngeal arch 6
ANSWER
16. Craniofacial syndromes often affect more than one pharyngeal arch. Which of the following clinical findings would indicate the involvement of pharyngeal arch 2 in this particular case?
A. absence of the malleus (as determined by radiography)
B. hypoplasia of the hyoid (as determined by radiography)
C. hypocalcemia
D. immunodeficiency
E. hypothyroidism
ANSWER
17. Which of the following could you expect to find upon further examination?
A. palatal abnormalities
B. maxillary abnormalities
C. hearing loss
D. NONE of the above
E. ALL of the above
ANSWER |